The mortality rate associated with suicide attempts involving ingestion of paraquat is alarmingly high, leading to its prohibition in China for production, sales, and use. As an alternative, diquat (DQ), a pyridine herbicide, has become prevalent in agriculture. However, despite efforts by the government to improve pesticide management and regulation, the number of cases of acute diquat poisoning caused by herbicides has continued to rise annually. The majority of patients suffering from DQ poisoning experience severe multiple organ failure, central nervous system injury, and circulatory failure during the acute phase, resulting in rapid and often fatal illness.
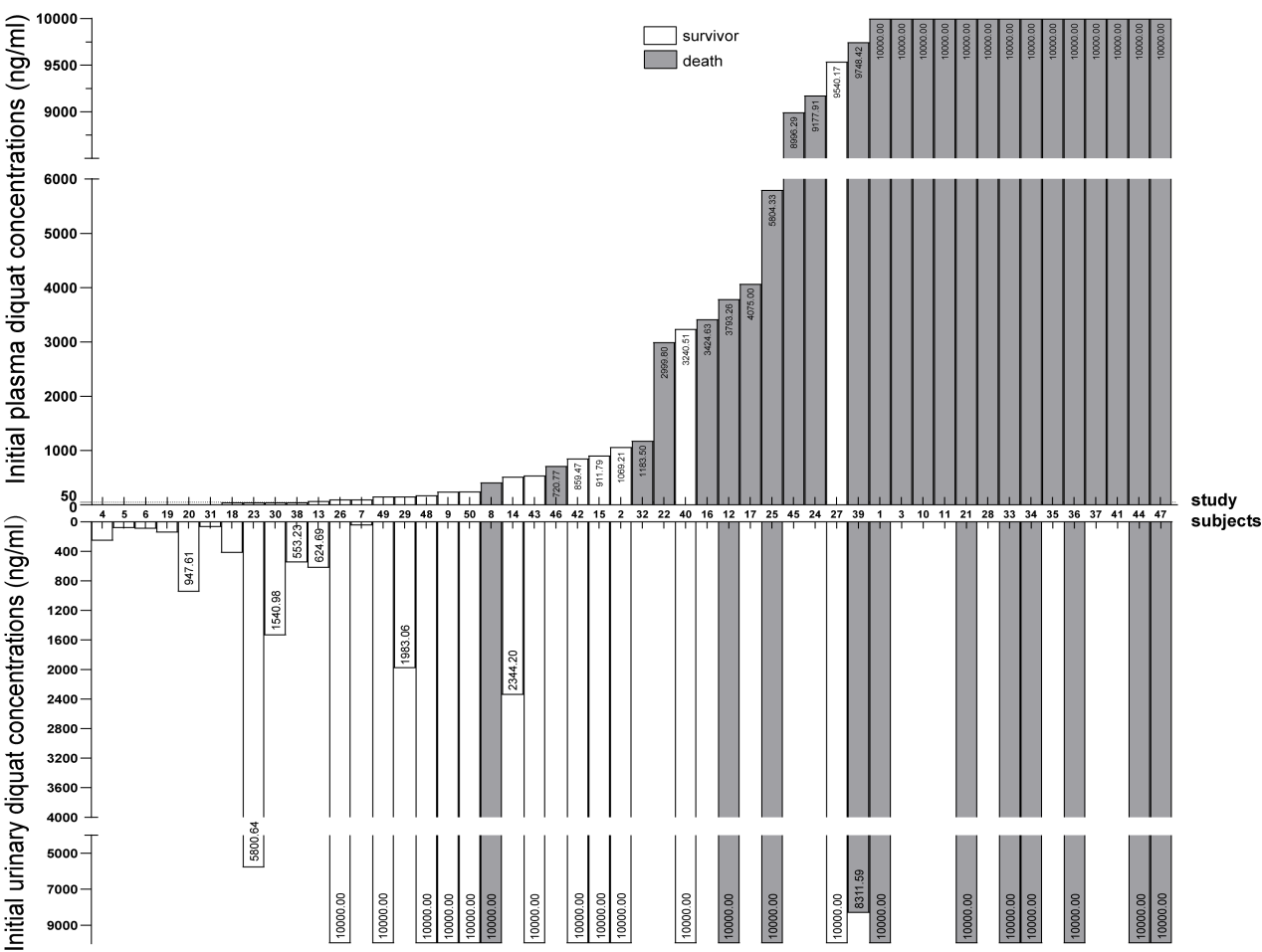
Figure 1: The prognosis of acute diquat (DQ) poisoning is related to the initial plasma DQ concentration
Prof. LU Yuan-qiang, director of Emergency Department of the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZU) published an article recently in eClinicalMedicine, entitled Lethal diquat poisoning manifests as acute central nervous system injury and circulatory failure: A retrospective cohort study of 50 cases. The study demonstrated a positive correlation between initial plasma DQ poisoning after admission and mortality in patients with acute DQ poisoning. The primary cause of increased mortality in patients with acute DQ poisoning is refractory circulatory failure, and the second is central nervous system injury in the brainstem region.
The initial plasma DQ concentration after admission is considered a well-detected indicator for assessing the specific DQ intake volume. It does not depend on the patient's medical history, which avoids bias caused by false recall and vomiting after taking medication. In addition, the convenience and accuracy of detecting plasma DQ concentration make it a promising indicator for evaluating daily therapeutic effect in patients with DQ poisoning. Professor Yuan-Qiang Lu's team proposed for the first time to predict the prognosis of patients with acute DQ poisoning through the first plasma DQ concentration after admission. This study found that central nervous system injury invariably preceded circulatory failure in acute DQ poisoning patients who developed central nervous system injury combined with refractory circulatory failure.
The mortality rate of acute DQ poisoning was 25 (50%) out of 50. Compared with the survival group, the death group presented significantly higher initial plasma DQ concentration, aspartate aminotransferase, alanine aminotransferase, serum creatinine, and creatine kinase-MB (P < 0.05). We found that six (24.0%) patients died of central nervous system injury, six (24.0%) patients died of refractory circulatory failure, and 13 (52.0%) patients died of central nervous system injury combined with circulatory failure. Receiver operator characteristic curve analysis showed that the area under the curve of initial plasma DQ concentration was 0.967 (95% CI: 0.911, 1.000), and the cut-off value was 3516.885 ng/mL (sensitivity, 90.9%; specificity, 96.0%). These results indicated that lethal DQ poisoning can ultimately lead to fatal complications of central nervous system and circulatory failure. Further research into the mechanisms of refractory circulatory failure and central nervous system damage could help reduce mortality.
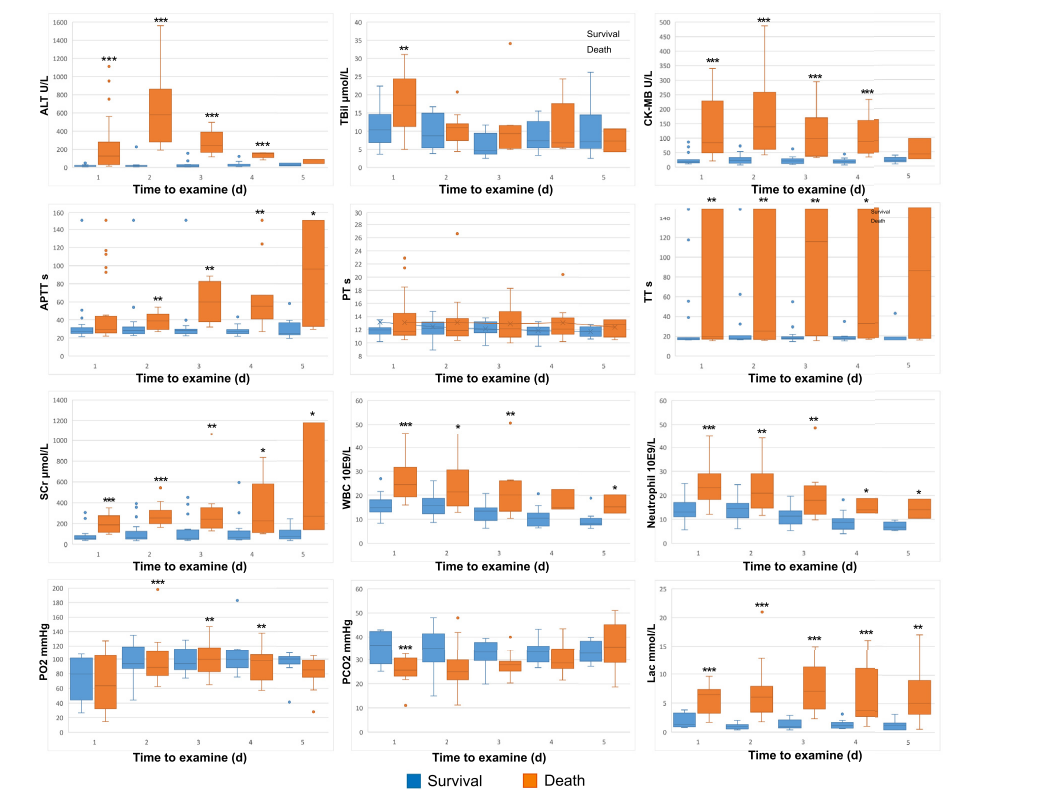
Figure 2. Clinical characteristics of acute DQ poisoning.
“Our research shows that plasma DQ concentration has been proven to be an efficient and accurate method for evaluating the therapeutic efficacy of DQ poisoning, especially in cases of lethal dose DQ poisoning. Professor LU comments that the current lack of effective clinical treatments for rescuing patients with lethal DQ poisoning underscores the importance of further exploring the mechanisms underlying DQ poisoning."
More information: Dr. ZHOU Jia-Ning is the first author, and Prof. Yuan-Qiang Lu is the corresponding author of this article.
Source: The First Affiliated Hospital, Zhejiang University School of Medicine


