Klebsiella pneumoniae, a member of the Enterobacteriaceae family, is a common pathogen in both community-acquired and healthcare-associated infections. Carbapenem-resistant Klebsiella pneumoniae (CRKP) is known as a superbug and antibiotic killer due to its complex enzyme profile and high virulence. According to data from the National Bloodstream Infection Bacteria Resistant Surveillance Network (BRICS), the detection rate of CRKP among bloodstream infection (BSI) isolates in China reached 19.2% in 2019. Currently, treatment options for CRKP infections are extremely limited, and the mortality rate among CRKP-infected patients is as high as 48%. Polymyxins, including polymyxin B (PMB) and polymyxin E, have become the last resort for treating CRKP infections, and it is crucial to further understand the resistance characteristics of CRKP to such drugs.
Recently, Prof. XIAO Yonghong’s team from the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZU), published a paper titled Clinical, biological, and genome-wide comparison of carbapenem-resistant Klebsiella pneumoniae with susceptibility transformation to polymyxin B during therapy in Clinical Microbiology and Infection, the official journal of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). The paper explores the drug susceptibility shift and resistance mechanisms of CRKP in patients undergoing polymyxin B therapy.
This study retrospectively collected relevant data from patients with CRKP infections receiving PMB treatment. Patients who experienced a shift from PMB sensitivity to resistance were categorized as the transformation group (TG), while those who maintained PMB sensitivity were classified as the non-transformation group (NTG). A total of 160 patients (37 in the TG, 123 in the NTG) were included in this study.The duration of PMB treatment before the appearance of PMB-resistant K. pneumoniae (PRKP) in the TG was even longer than the entire duration of PMB treatment in the NTG. Compared with isogenic PMB-susceptible K. pneumoniae (PSKP), most PRKP strains had missense mutations in mgrB (12 isolates), yciC (10 isolates), and pmrB (seven isolates). The competition index of 82.4% (28/34) of PRKP/PSKP pairs was less than 1. In addition, 67.6% (23/34) and 73.5% (25/34) of PRKP strains showed a higher 7-day lethality in Galleria mellonella and a greater ability to resist complement-dependent killingthan their corresponding PSKP, respectively.
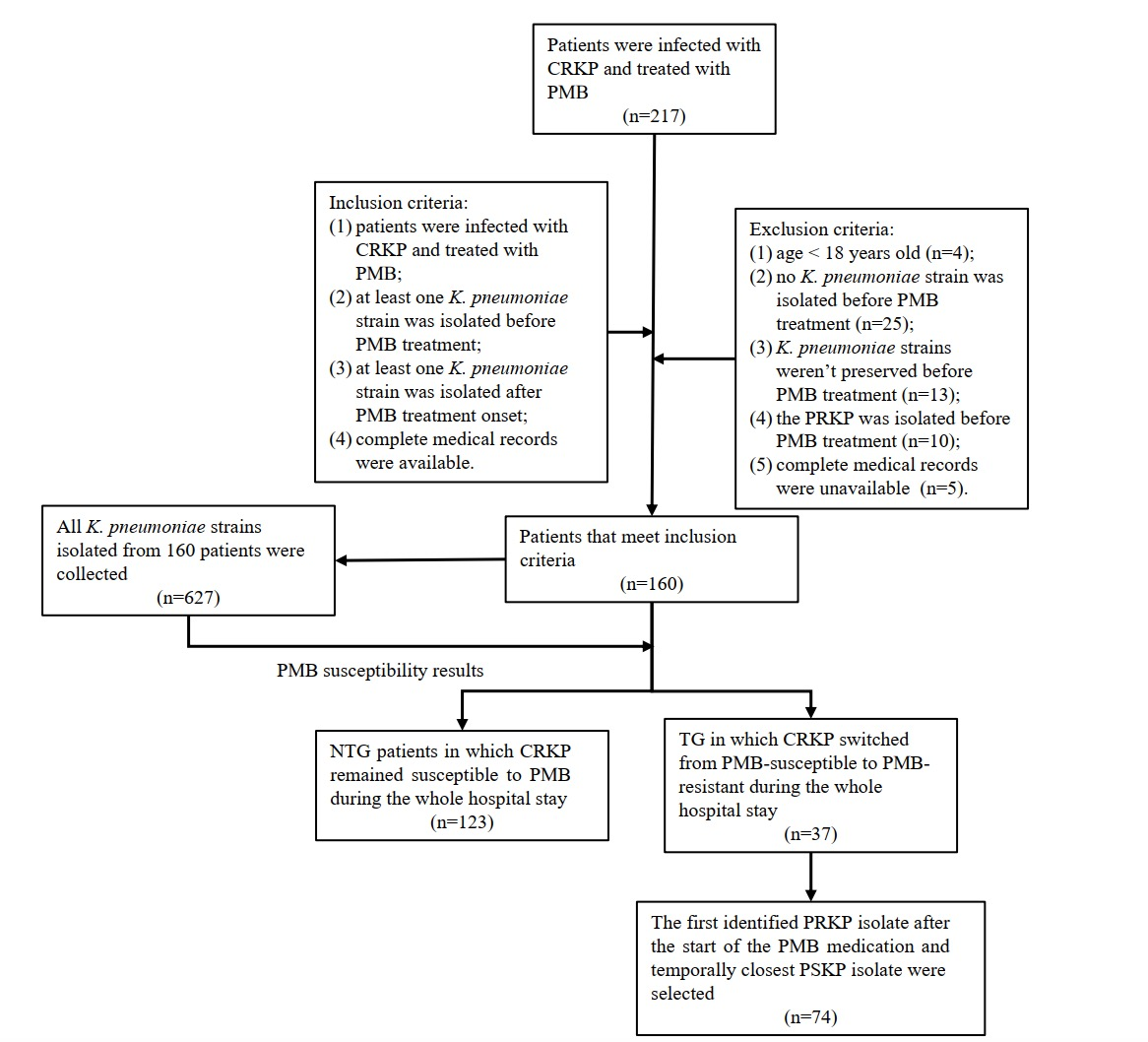
Figure 1. Flowchart showing study inclusion and exclusion criteria.
The results of this study indicate that infected patients with CRKP are prone to developing polymyxin susceptibility transformation after PMB treatment. The emergence of polymyxin resistance may be explained by suboptimal dosing of PMB and its long-term use. The evolution of PSKP to PRKP is mainly driven by gene mutations in mgrB, yciC, and pmrB. Strains that evolved from PSKP to PRKP exhibited reduced growth and increased virulence. These findings suggest that prudent use of PMB is required in the clinic, including appropriately increasing the dose to avoid prolonged use and prevent the emergence of resistant bacteria.
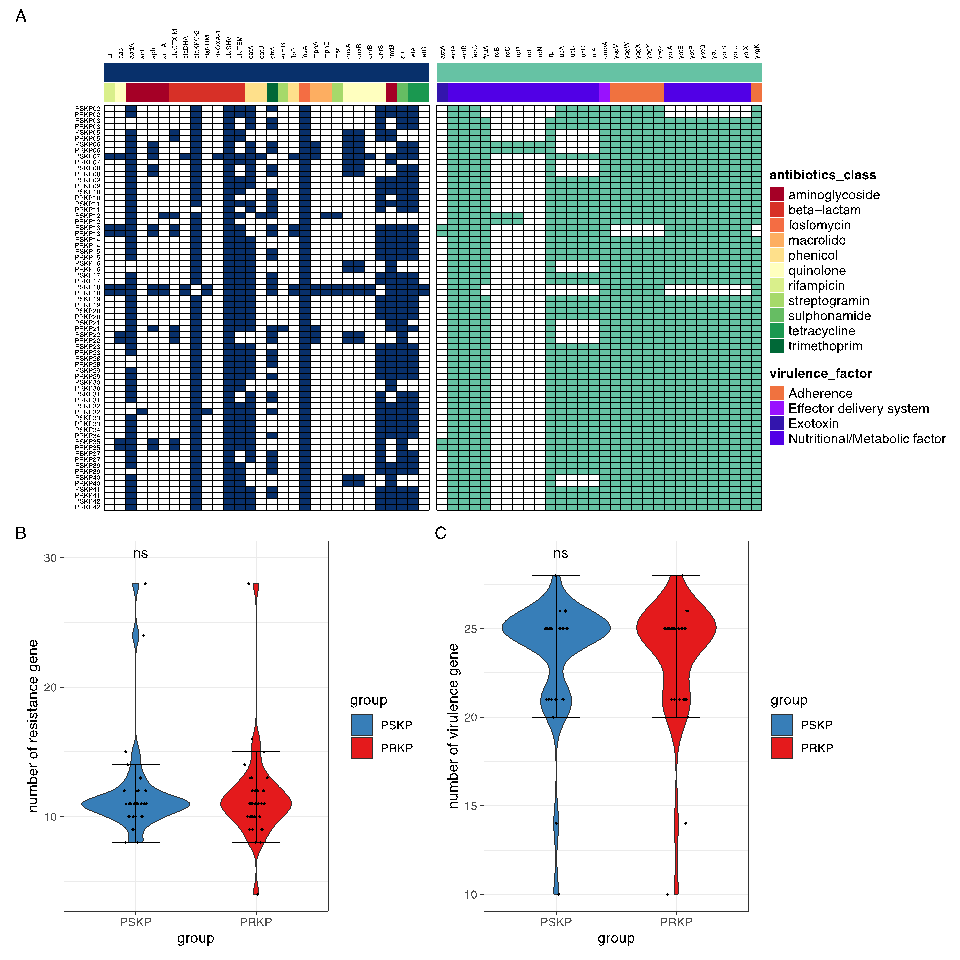
Figure 2: Distributions of resistance genes and virulence factors in 34 pairs of PSKP and PRKP strains in the TG.
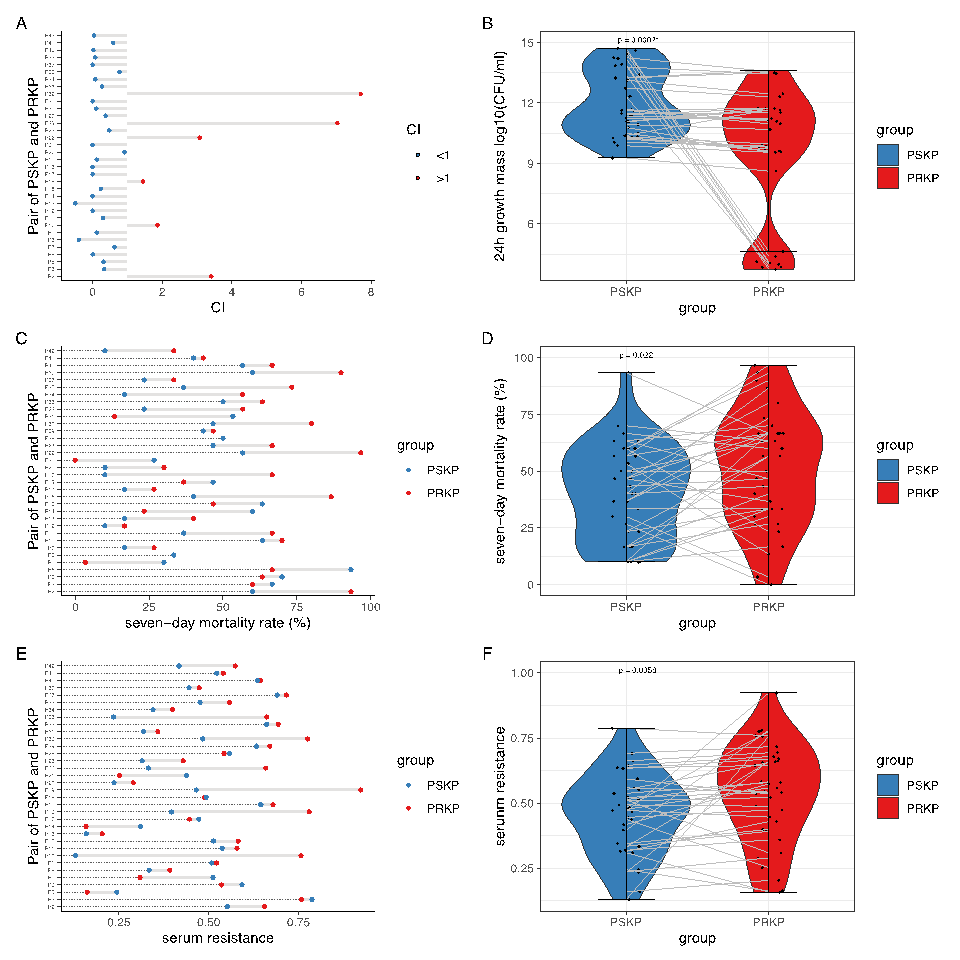
Figure 3. Fitness and virulence of 34 pairs of PSKP and PRKP in the TG.
Prof. XIAO stated that polymyxins are one of the limited treatment options for combating carbapenem-resistant Gram-negative bacteria (CRO) infections in China. However, the sensitivity shift or acquired resistance during treatment can further reduce the effectiveness of polymyxins and increase the risk of dosage escalation and adverse reactions. In this study, 23.1% of the enrolled patients experienced a transformation from susceptible to resistant during polymyxin B treatment, indicating that approximately one-fourth of the patients acquired resistance during the course of treatment and highlighting the need for clinical attention. It is evident that longer treatment duration and lower drug dosage exposure may contribute to the occurrence and development of polymyxin resistance. Therefore, the clinical use of polymyxins should align more closely with professional requirements.
More information: WANG Yuan, CHEN Tao and CHI Xiaohui are the co-first authors of this article. Prof. XIAO Yonghong and Dr. LUO Qixia are the co-corresponding authors of this article.
Photo credit: the research team led by Prof. XIAO Yonghong.


