Bipolar disorder is a severe and disabling psychiatric disorder with the potential for adverse outcomes, such as suicide, if patients do not receive standardized therapeutics. The most commonly used pharmacotherapies for bipolar disorder (BD) are antipsychotics and mood stabilizers, which may cause metabolic abnormalities such as insulin resistance and hyperlipemia.
Recently, Prof. HU Shaohua’s and Assistant Researcher LU Jing’s team at the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZU) published a network meta-analysis titled "Effect of antipsychotics and mood stabilisers on metabolism in bipolar disorder: a network meta-analysis of randomised controlled trials" in eClinicalMedicine.
This network meta-analysis involved 41 publications (Fig. 1). In total, 17 antipsychotics and mood stabilizers were analyzed and ranked according to their effect on glucose metabolism (fasting serum glucose, serum insulin, HbA1c), lipid metabolism (total cholesterol, total triglyceride, LDL, HDL), anthropometric measurements (body weight, BMI, waist circumference), serum prolactin, and total serum bilirubin (Fig. 2). Subgroup network meta-analyses of age, sex ratio, current episode, race, intervention duration, and baseline medication were also performed to determine the metabolic effects on BD patients with different characteristics.
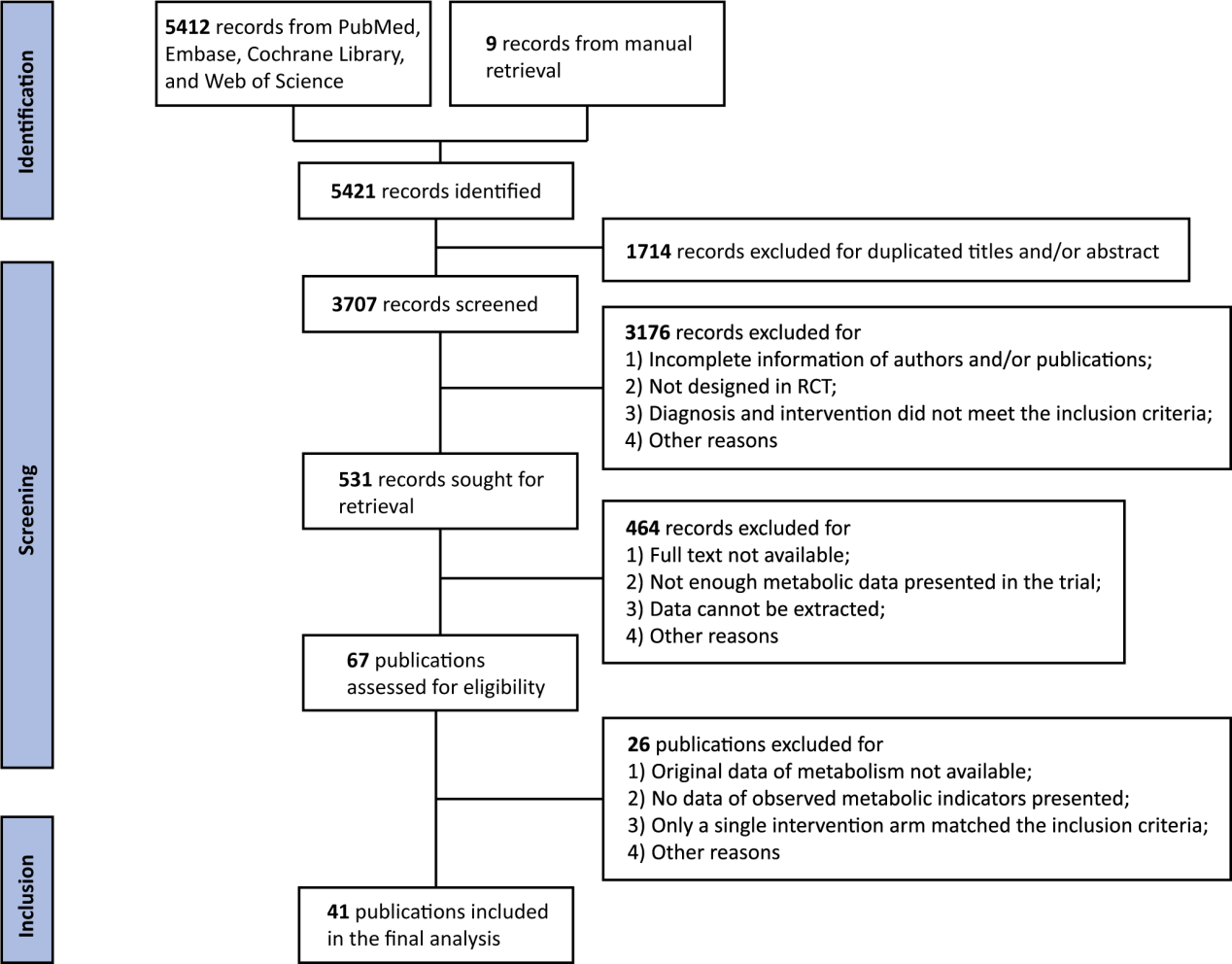
Figure 1: Flow diagram.

Figure 2: Network maps and league tables presenting head-to-head comparisons of fasting serum glucose, TC, TG, and body weight.
Antipsychotics are more likely to disturb metabolism than mood stabilizers and placebo. The general ranking was based on the rankings results from five representative indicators (fasting serum glucose, TC, TG, LDL, and body weight). Olanzapine ranked the highest in elevating these metabolic indicators, while mood stabilizers ranked below placebo. In addition, the newly-approved antipsychotic, lumateperone, showed fewer metabolic effects (Table 1).

Subgroup analyses indicated that quetiapine is more likely to affect glucose metabolism among male adults with a current episode of bipolar mania/hypomania or mixed state and with baseline medication, while long-term lurasidone tends to affect glucose metabolism among female patients with bipolar depression. Moreover, among the youths, divalproex tends to affect glucose metabolism, while lithium shows stronger influence on lipid metabolism.
Furthermore, efficacy (response rate and remission rate) and tolerability (dropout rate) analyses were also performed based on the applicable data retrieved from the involved publications. According to the results, most antipsychotics perform better in terms of efficacy than placebo and are also tolerable, except for olanzapine.
The results of the network meta-analysis provide evidence-based information and clinical inspiration for drug compatibility and further research on the mechanisms of BD. Attention should be paid to individual applicability in clinical practice.
More information: The co-corresponding authors of this study are Professor HU Shaohua and Assistant Researcher LU Jing from FAHZU. The first author is KONG Lingzhuo from the Class of 2022 at FAHZU. The co-first author is WANG Huaizhi from the Class of 2022 at Wenzhou Medical University.


