Chyle leak (CL) following pancreatectomy primarily results from iatrogenic injury to the cisterna chyli or its tributaries during pancreatic resection procedures. Having been overlooked for decades, CL has increasingly been recognized as a clinically relevant morbidity following pancreatic resections. It can result in malnutrition, lower immunity, and secondary infections.
In 2016, the International Study Group for Pancreatic Surgery (ISGPS) introduced a definition and classification system for CL. The ISGPS classifies CL into grades A, B, and C according to the management needed. For the first time, a universal and objective definition and classification system for CL following pancreatic surgery has been established, allowing the valid assessment and comparison of studies across different institutions. However, the ISGPS definition on CL following pancreatectomy has not been fully validated.

Prof. Liang Tingbo’s team from the First Affiliated Hospital, Zhejiang University School of Medicine(FAHZU) reappraised the validity and clinical utility of the ISGPS definition and classification of CL after pancreatic surgery. In this study, the validity of the ISGPS classification of CL was confirmed. However, the current definition may omit a large proportion of patients whose postoperative triglyceride (TG) concentration of the drain was over 1.2 mmol/L without a milky-colored appearance. This study highlighted that post-pancreatectomy patients with large-volume, TG-rich (≥1.2 mmol/L) but non-milky drains should be treated like clinically relevant CL. This study was recently published in Annals of Surgery.
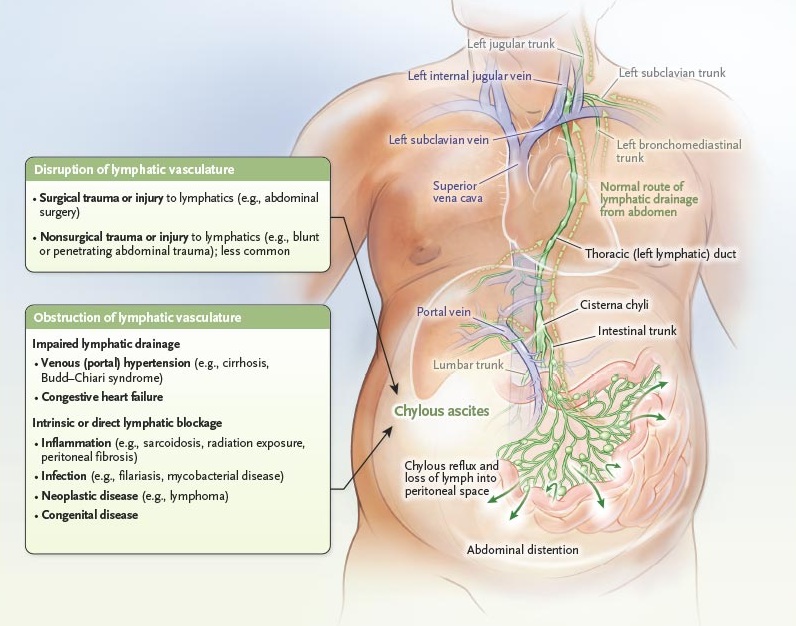
Photo Credit: The New England Journal of Medicine
The authors emphasized that the clinical significance of CL lies in the substantial loss of triglyceride-rich lymph, which may lead to metabolic depletion and systemic inflammation. Quantitative measurements of drainage volume and TG levels provide more objective diagnostic criteria than relying exclusively on drainage appearance for the early detection of clinically relevant CL. This study highlights the critical need for incorporating drainage volume parameters into current diagnostic models.
More information: The work’s co-first authors are LI Huiliang, MA Tao, and LIN Wei-chiao from the First Affiliated Hospital, Zhejiang University School of Medicine (FAHZU). Prof. LIANG Tingbo and MA Tao from FAHZU are co-corresponding authors.


